PMHx: no previous lung Dz. +CAD, S/P PTCA.
SHx: never smoked. Retired from management position. Current hobby is to work with rare woods and make pens. He always wears a mask. No use of Western red cedar.
On exam, AAOx3. Good dentition. Decreased BS R base with crackles, egophony and dullness. S1/S2 RRR. Benign abdomen.
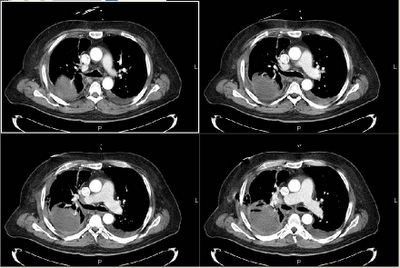
CT scan is seen below.
Besides comments on management and next step, what is the practice at your institutions RE: infusing thrombolytics via CT for empyema?
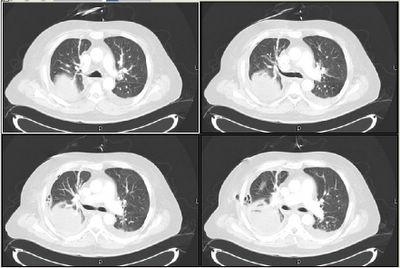
Same level (lung windows):
7 comments - CLICK HERE to read & add your own!:
Does it look like a vessel is going in there? It looks like there is a consolodation and then the thick pleura and then fluid (pleural effusion) posterior to that larger collection. It also looks like that larger collection has an airfluid level. Maybe the abcess. He obviously has a very loculated effusion now which leads to my first question: After the 1st tube was placed, was there complete resolution/drainage? How long after his presentation was the tube placed? How long do you think he had the effusion prior to getting it drained? It sounds like he now has a chronic loculated effusiuon because of the original empyema being there for long enough to cause pleural fibrosis.
The management would be surgical, with decortication.
As for the thromolytics, we have done that at our institution. I suspect this will be less with the NEJM article suggesting it's less-than-usefulness. One caveat to that study, though, was that the chest tube size was like 12 french or something really small. But I think Horowitz or someone had mentioned that when they stratified by tube size there still was no difference.
Yea, the posterior aspect does not look like a pleural collection; it looks like a parenchymal abscess with an air-fluid level. It's in the right base, so I'd wonder if he has a problem with aspiration-concern for anaerobes. Also, this could easily be a necrotizing pneumonia due to Klebsiella.
There is, on the lung windows, what looks like some air in the pleural space on the right-possibly some in the right chest wall as well. Was this CT done after a thoracentesis? Although it doesn't really look like the fluid collection is "invading" the chest wall, I'm keeping Actinomyces in the back of my mind.
The actual pleural fluid collection doesn't look that impressive. It could be reactive, or may be pleural thickening/fibrosis from the prior empyema. Is it free flowing? If it is a recurrent empyema (or one that failed to fully resolve the first time), than I agree he needs surgical intervention. He would need an empyema tube at the very least, and possibly a decortication if his lung function is comprimised.
For the abscess, the treatment is long-term antibiotics. Clindamycin is best studied, although Unasyn/Augmentin is probably just as good. There is some recent literature regarding drainage with pigtail catheters, but I think the risk of a abscess-pleural fistula and chronic empyema makes this a risky option. I'd give at least 3 months of antibiotics--sometimes these will need more than a year.
With regards to thrombolytics, I saw little use for them prior to the most recent NEJM paper; I see even less utility in using them now.
Jeff H raised some great points about the air-fluid level and the tracking into the chest wall. He did have a previous chest tube at the OSH giving it almost the aspect of an empyema necessitans. Since he had been on ABTx I chose to go for gusto and started Zosyn and Vanco (for possible contamination with MRSA @ OSH) until Cxs became available. I'll post some follow-up once everyone has had a chance to check it out.
I was going to mention things like actinomycetes,but I thought he was deliberately leading away from that when he mentioned the good dentition.
BTW, when you post the "answer", do it under the comments in THIS post and then make a new pot that simply contains the link back here. That way, when we or others go back to the archives, each case can be read en toto with the answer revelaed as the last comment. Also, if the answer (or followup) is in a separate post, it would be a nightmare for searching...
I may have been led astray by the "good dentition," except that I failed to see it when I read the post the first time.
Carlos--are you treating for an abscess or for suspected empyema?
We have had the same dilemma outlined by Jeff H: empyema with a very complicated space vs. pulmonary abcess with pleural compromise...
He was admitted to the CT surgery service so we proceeded as dollows:
1-Drained fluid and placed a pig-tail cath so we could repeat the CT scan and re-think. Fluid was purulent with pH 6.0 (done in lab, not immediatelly wit strip...), 3.5 million WBCs (all PMNs), LDH >43,000, glucose <20 and protein 4.0. Gram stain showing GPCs and GNRs.
2-Based on Gram stain (and I WAS trying to lead you away from Actyno, his teeth are actually in very good condition) we kept him on vanco and Zosyn while Cxs pending.
3-Prior to further exploration, he had a cardiac cath and a critical LAD lesion was stented in anticipation of surgery.
I will post the post-pig-tail pictures on Monday and try and wrap it up.
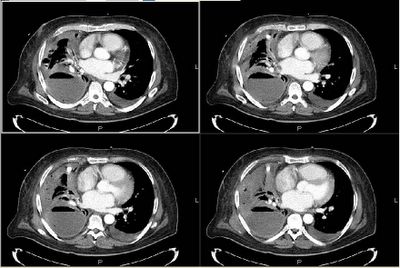
After drainage through the pig-tail catheter he has had marked symptomatic improvement. Pleural fluid cultures grew alpha-hemolytic Strep and Bacteroides fragilis. He is still on Zosyn. As you can see on the scans the major fluid pocket on the left is completely resolved (with thickened pleural and areas of air-space consolidation). He is still going to have surgical decortication but at cardiology's request this will be delayed so he can stay on Plavix/ASA a little longer to prevent hyper-acute stent closure.
I will close this post as mixed flora empyema in the setting of previous chest tube for empyema. Perhaps surgical evaluation during his initial presentation to the OSH would have prevented this progression. If there are any new scans or events I will post them as a separate post at a later time.
You can see this follow-up post (with CT images) as http://pulmonaryroundtable.blogspot.com/2005/06/follow-up-to-pleural-disease.html
Post a Commenttest post a comment