see the original case. I will also edit the original case to include this, but comments should be added here.
I was called by a prominant chest radiologist before I saw the patient. He told me that the patient had a left lower lobe pneumonia and possibly some central bronchiectasis. So, combined with his spirometry, I obtained studies to evaluate for ABPA (these were negative) and gave a burst and taper of prednisone for his untreated asthma. Because, clinically he had nothing to suggest a pneumonia, I ordered a CT scan.I saw him back in clinic 2 weeks later.
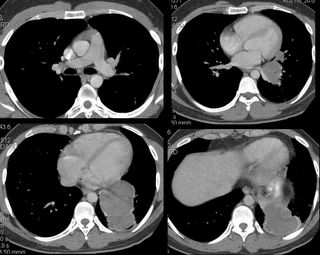
His PFT's had improved significantly:FEV1 up to 2.6 L (from 1.78). FVC was unchanged. His TLC was 74% predicted, and his DlCO was normal. His CT scan is shown:
So, now what?
PART 3:
We thought, given the mild eosinophila, his immigration history, and the cystic appearence on CT scan with what appeared to be multiple septae, that this could very well be an echinococcal cyst. Other possibilities included malignancy (esp sarcoma), or sequestration (although we did not identify a feeding vessel). I did not show it, but there was one 2 cm calcified lesion in the liver. So, I presented his case to thoracic surgery for primary resection. Our surgeons asked for an ID opinion, which was obtained. Although review of the literature showed that percutaneous drainage may be an option for hydatid cysts in the liver, this has not been shown in the lung. The ID consultants agreed with primary resection, but we chose to treat for 3 months with albendazole first.
Two weeks later, the story changed again. I was contacted by another radiologist (who had seen the initial CT scan in a conference). She sent me some computer reconstructions:

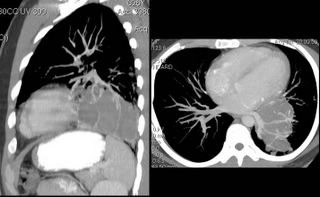
As seen, what we thought were septations were, in fact, vascular branches off of the left pulmonary artery. Additionally, she felt that the fluid density was not cystic (60 hounsfeld units). Now, the possibility of sarcoma came into play.
CONCLUSION: I showed these films to our thoracic surgeon, who again balked, so I rephrased the question. I asked him to name any potential diagnosis of this lesion for which resection was not appropriate management. The patient was taken to the OR 2 weeks later, and a left lower lobectomy was done.
Gross Path: multiple cystic lesions containing "thick green and brown material."
Microscopic Diagnosis: bronchiectasis with eosinophilic abscesses.
There were no parasites seen. There was no fungus. Cultures were negative.
I saw the patient in follow-up last week, and we are both dissapointed at the lack of a definitive etiology for all of this. He feels well, although he stopped taking his meds and his airways obstruction has significantly worsened. He is off of the albendazole, and we have chosen to follow-up clinically and with periodic imaging to identify any potential new lesions at an early timepoint.
Any other comments, thoughts, or suggestions?
9 comments - CLICK HERE to read & add your own!:
Well, I am glad I could still see that on the CxR even at lower size. The structure apperas cystic, fluid-filled. Pulmonary sequestration could look like thata. It should not lead to the relative eosinophilia but it seems to be pushing against bronchi leading to partial obstruction and bronchospasm. We don't have lower cuts but it does not look like a diphragmatic hernia.
I don't see a "double-crescent" but I see a small crescent posteriorly. So, to stay in the realm of esoterica with his travel history I will add hidatid cyst (echinococcosis) to the differential: it would cause the cystic lesion, eosinophilia and local bronchial compression/obstruction.
Anyone else have any input here? I'll add the next update tomorrow, but if there's no interest than I'll just end it.
I know the case that's why I haven't commented. Go ahead and post the answer (in a new post with a link to this one).
So what happened to DK, MM, and ML? I'll finish up the case tomorrow.
Yeah, not sure what's up with that. Ok tomorrow it is...
When CB gives his differential diagnosis first, it is hard to think of anything else to add.
I did see that abnormality on CXR, but thought it was a function of my monitor being lousy.
I assume you have some sort of tissue analysis to determine the etiology...
We anxiously await.
I left out other cystic lesions such as pericardial and bronchogenic cysts. Because of resolution and number of cuts (Jeff, I'm not complaining, just making up excuses) I cannot follow the lesion well to see whether it is indeed continuous with some of the other structures around. On the second image (right upper) it seems very close to the bronchus with a thick posterior density suggesting it is pushing away part of the pulm artery to that area. I guess a bronchogenic cyst could explain it all and would be simpler than echinococcosis (though less exciting).
Teratomas can be cystic (like other germ cell tumors) but I would expect it more anteriorly and more mixed densities. Finally, there is a mucinous type of bronchogenic Ca that can be very cystic-like but I don't remember if it can happen in non-smokers (5 years of 3 ppw in TN is a non-smoker) similar to bronchoalveolar.
Post a Commenttest post a comment