Jeff H had suggested a PET. We were discussing the timing of a PEt and f/up with CT surgery when the patient came in through our ED this past Sunday with worsening dyspnea, cough (non-productive) and a fever to 104. This presentation is now only 20 days from that most recent CT scan on the previous post.
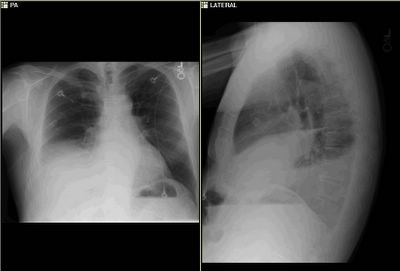
His CxR showed the following:
I performed a thoracentesis and the fluid was turbid yellow with a lot of sediment. LDH was ~ 9,000, protein 4.3, glucose <10 and there were 17.9K WBCs with 97% PMNs. Gram stain showed WBCs but no organisms.
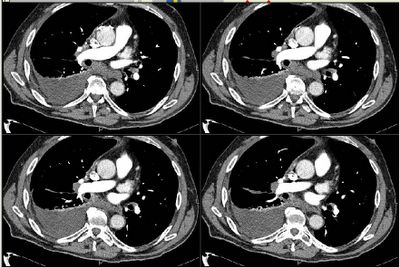
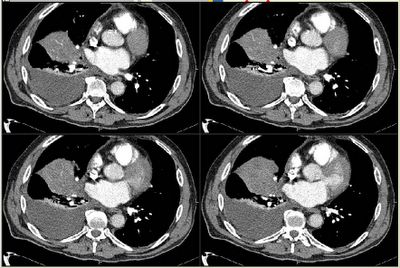
His new CT scan looks like this:
Now what?
3 comments - CLICK HERE to read & add your own!:
So, now I really think the initial lesion was actually in the pleural space/fissure. Now, there is a large collection in the pleural space, posteriorly and in the minor fissure. It's strongly exudative, with no bugs on gram stain. I don't see clear loculations, but it may be a complicated parapneumonic effusion.
My question no is: how much fluid were you able to tap, and how free flowing is this. It's density looks very much like soft-tissue, and I now think that mesothelioma is a distinct possibility.
If this were lobar collapse, I'd expect the fluid to be transudative or, at least, not strongly exudative. The characteristics are not c/w a tuberculous effusion. Was it chylous?
So, my differential now is complicated parapneumonic effusion (? due to a malignancy and post-obstructive pneumonia), vs. pleural malignancy-(mesothelioma or, less likely, pleural metastases).
I'd treat with antibiotics for CAP but also cover anaerobes (i.e. Unasyn/quinolone or Unasyn/macrolide), further evaluate the characteristics of the fluid (free flowing vs. loculated vs. not much fluid and a lot of soft tissue), and proceed with repeated large volume thoracentesis with a consideration of chest tube placement. If it is loculated or contains more soft-tissue characteristics, I'd push for a VATS to examine/biopsy.
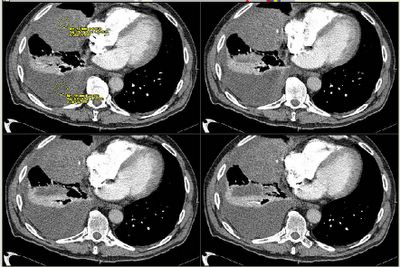
um, I can't really add anything to what horowitz said. I assume the yellow markings were to indicate that the hounsfield units were similar and thus that the original "mass" was fluid in the fissure. One of the slices sure seem to indicate that and looks like they also communicate with the mediastinal space - it is this last point that may have led horowitz to think about mesothelioma.
Very good points. Jeff H's pick up on location was along the lines of what we were thinking. It seems that there was a fissure based process now secondarily infected.
I was only able to drain ~300 ml but the post-thoracentesis film showed almost complete resolution of the effusion (?) with obvious persistence of the RML process.
The fluid was free-flowing but with a lot of debris. I chose Zosyn and Levaquin for his empiric ABTx. He is now afebrile.
The measured units don't come across as well on the posted pic... the effusion is around 0-14 HUs consisten with fluid but the pulmonary process is more heterogeneous with average densities 30-40 HUs.
He is clinically improved and will go to CT surgery tomorrow to sample and clean up the pulmonary process and the pleural space.
I will try and post an update tomorrow.
Post a Commenttest post a comment