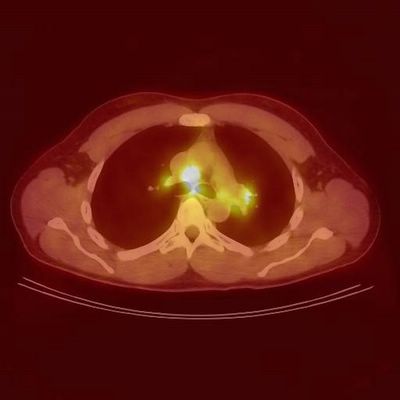
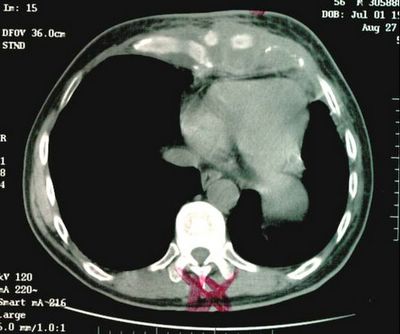
So I agree with the two comments that you don't biopsy a lung nodule in an otherwise good surgical candidate, which this man was. He of course went on to receive chest wall radiation starting two weeks after his surgery and finishing in late July 2000, which is of course why I met him in September of 2000, about two months after completing his XRT. He had a mild case of radiation pneumonitis with dyspnea, and cough. I treated him with steroids for about 9 months because of a tendency for relapse when I tapered him. He was then doing well for about a year, when he came back to see me becuase of a CT showing mediastinal and hilar adenopthy. He had two unseuccessful attempts at Wang needle bx including a very large pre-tracheal LN, because of this I referred him for a mediastinoscopy, but first ordered another PET to see if he had any other evidence of distant disease (PET LN jpeg file below). When he returned to see me to discuss the PET a week later he complained of some redness and pain on his anterior chest wall which I treated as cellulitis.He was set up for a mediastinoscopy, but when he presented for this appointment 5 days later, he complained of increasing pain and redness over his anterior chest even after taking Cephalexin for the last week. He had an admission CXR that showed a large soft tissue density and had the following CT scan the day of his planned mediastinoscopy. (9-02 chest wall image below). Now what would you do?
Answer posted in the discussion below.
3 comments - CLICK HERE to read & add your own!:
This case keeps getting sadder.
I would ask the surgeons to biopsy the chest wall mass that is present on the CT scan.
How soon after the PET scan is the CT?
Same question Re: the time between the 2 studies. There was not much on the chest wall in the PET-CT image so the mass on the second study could be inflammatory/infectious in nature (though with all the PET+ areas and the previous Hx that might be wishful thinking).
I agree with the chest wall biopsy for the possibility of infection. However, presumably this is a recurrence- however, chest wall invasion would not definitively exclude surgery, as (ignoring for the moment the pre-tracheal light-bulb on PET). So, if this patient would otherwise be a surgical candidate, the mediasteinoscopy would still be necessary for definitive staging.
Post a Commenttest post a comment