PMH was significant for a cadeveric renal transplant that had been done 23 (yes, twenty-three) years previously for reasons entirely unrelated to her current presentation.
The remainder of her history is non-contributory.
Pertinent medications include: Cellcept 500mg BID, Prednisone 8 mg QOD
A CXR was done:

Notably, 5 weeks prior to this presentation, her CXR was normal.
A CT scan was done:
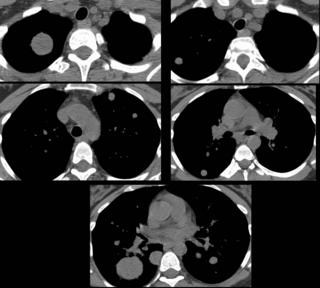
In all, I counted 17 of these nodules and masses. Morphologic and attenuation patterns were all similar, although the sizes were quite variable.
So, what is the differential diagnosis and diagnostic approach.
I will respond and update as some comments come in.
Answer posted below in the comment section.
8 comments - CLICK HERE to read & add your own!:
watch it, bubba.
Anyway, I do agree that infectious seems to be the most likely; lack of symptomatology is unusual, but then it would be unusual for almost anything on the differential. Also, her immunocommpromised state means she is susceptible to infections. On that note, I might think that an autoimmune etiology is less likely because she is immunocompromised. Cancer, via hematogenous spread is less likely given the rapidity, and it doesn't look like the more rapid cancers like small cell.
Bronchoscopy was non-diagnostic. All serologies were negative. All labs were normal. A CT guided biopsy was non-diagnostic (all ghost-cells and necrotic tissue).
What, if any, infections and/or neoplasms might be likely?
Those are very impressive. Being on immunossuppression this long not only puts her at risk for infectious complications such as Aspergillus (even if she is not neutropenic) and TB but also for malignancies (though they seem to have grown awfully fast) such as lymphomas and solid organ tumors (some sarcomas can appear to grow fairly fast).
I'd ask the CT surgeons to try and get a VATS Bx of one of those.
Do we know which regimens she had been on in the past? PPD status?
Nocardia can present this way - either by direct inhalation or hematogenously.
I agree that sarcomas may fit the bill in someone on immunossup. for such a long time.
That was our thinking. The short list consisted of Nocardia versus post-transplant lymphoproliferative disorder and/or lymphoma, with less likelihood of endemic fungi or aspergillus. We were also concerned about the possibility of metastatic disease (possibly arising from one of her native kidneys).
All cultures from both the bronch and from the CT guided core remained both smear and culture-negative.
A CT scan of the abdomen and pelvis showed no evidence of masses or lymphadenopathy.
So, the question now is: would you initiate (or would you have initiated) any empiric therapy prior to any of the biopsies or now while arranging for a VATS? If so, what would you start?
I will post the follow-up after giving some time for final comments.
I think I'd have a lower threshold to start antifungals and ABTx. She has been sick for a while and is likely to get worse before she gets better... especially if she has fungi in there.
She was initially started on Voriconazole and Bactrim, but these were discontinued when the cultures remained negative. Following her CT-guided biopsy, she was discharged home. A repeat CXR done 3 days later showed enlargement of the nodules.
5 days after her CT guided biopsy, a VATS was done, with wedge resection of two of these nodules.
Path: numerous large B-cells (+ for EBV staining) diagnostic of PTLD/large B-cell lymphoma.
Post a Commenttest post a comment