PAST MEDICAL HISTORY: Allergic rhinitis and Asthma.
OCCUPATION: Distribution clerk at a post office for 21 years. No occupational exposures.
SOCIAL HISTORY: No tobacco. The patient has always lived in Michigan. No TB
exposure. No alcohol. No illicit drug use.
PHYSICAL EXAMINATION: Height 5 feet 7 inches, weight 230 pounds, blood pressure 152/73, pulse 91, and respirations 16. General: No acute distress. No cervical lymphadenopathy. Lungs: Clear to auscultation. No clubbing. Intact radial pulses
bilaterally.Abdomen: benign. No c/c/e
PFT's FEV1 1.84 (64%) FVC 2.42 (65%) ratio 76 (97%) TLC 3.61 (66%) Diffusion 72%
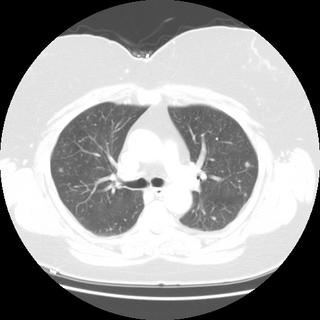
Review of chest CT revealed multiple pulmonary nodules; two representative slices are shown here:

DDx and other tests?
10 comments - CLICK HERE to read & add your own!:
She has a mixed defect with a BMI of 36.
Does she a have many other nodules? Any skin rashes?
How about a CBC with diff and IgE for starters?
Basically she either has straightforward asthma and now has a new infectious/inflammatory process or another condtion has been labeled as asthma all along.
I don't see any bronchiectasis in the cuts shown but she could have ABPM. Sarcoid could tie in the nodules and obstruction. She is a non-smoker so Lung Ca is low on my list but she could have metastatic Dz (e.g. medullary thyroid, etc.).
I get a sense that the nodules are not associated with an acute wrsening of her clinical course and since she has not had a previous CT, they have probably been there for a while so they may be related to the underlying condition that has been treated as asthma. Maybe she has HP in response to the moldy paperwork in the post office...
I agree with Carlos. One mimic of asthma would be Churg Strauss with some vasculitis leading to prior hemoptysis and some focal areas of ground glass nodules now. ABPA/ABPM is possible, and cancer is unlikely.
Maybe it is the resolution on my monitor, but there appear to be small nodules in addition to the larger ones.
I would put malignancy somewhat higher on my list than previously mentioned. She is in her late 50's, so she is at risk for colon cancer (especially distal colon/rectal cancer metastasizing to the lung in the abscence of liver mets), lymphoma, breast cancer and renal cancer.
Has she had her screening studies (mammography, pap/pelvic, colonscopy)?
Other things that can do this are AVM's.
Oh, and I would place a PPD. If this blog has taught me one thing, TB shows up in all kinds of unexpected places.
I can't access the computer until tomorrow to answer some of your specific questions. I will say that the decision was made to do a core needle bx of one of the bigger nodules (mendez was correct regarding multple nodules some smaller than others). That showed "necrotizing granuloma".
Any additional thought now? I'll fill in the rest tomorrow when I get back to the computer.
Her percent eosinophils was 2%. They did not send off an IgE though. It is true, as you guessed, that there was no bronchiectasis on the rest of the CT cuts.
Her histoplasmin Ab was positive (H band); blasto, coccidio and aspergillin Ab was negative.
The sputum had "rare mold, identification to follow" but there was also some candida and oral flora in another sample, so interpret with caution.
No HP panel was sent.
Hmm...I just noticed that they did not bronch the patient, so I can't give you a cell count.
As for wegeners, C-ANCA was negative.
As for Churg Strauss, P-ANCA was also negative.
I do not know about her screening tests; no GI symptoms at least, for what that's worth.
PPD was negative.
sed rate 25 and Creatinine 0.7.
U/A no blood protein, WBC's.
Hmm..interesting. Do you think the positive histo Ab in this patient is a red herring?
Doug-
Why methotrexate when there is an article using azathioprine in patients with stable WG after 4 months of CTX and prednisone?
Jayne et al. NEJM, Jul 2003; 349: 36
Post a Commenttest post a comment