
The next day his WBC was 30,k and on the 3rd day it was 45,000. He became more hypoxic. He remained normotensive. His cxr is shown here:
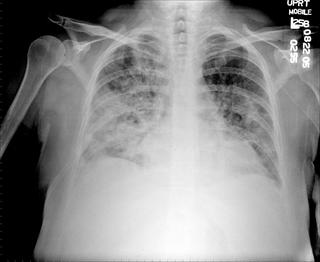
What might be the cause of the CXR findings, in the setting of this presentation?
Discussion of interesting or befuddling cases related to pulmonary and critical care medicine.

12 comments - CLICK HERE to read & add your own!:
In the first part of the case, is that WBC 9K or just plain 9?
The rapid radiographic changes coincide with WBC reconstitution as would be expected: as the marrow recovers, WBCs responsible for inflammation/pneumonitis arrive in the lungs.
The seconde CxR has B/L alveolar infiltrates (R>L) with increased interstitial markings as well and what appears to be an early cavitation/area of centra lucency in the R lung (without the lateral it looks like RLL but could be RML).
There is a very large differential here. The first major divide is whether this is an infectious process or not.
Infections are an obvious concern in this neutropenic patient: he has been on ABTx, probably had an ongoing infection and the infiltrates blossomed with marrow recovery. Fungal infections (Aspergillus) would be a big concern given the previous ABTx. I would have a low threshold to start anti-fungals though the marrow recovery is a good prognostic indicator. A CT scan would be very helpful to look for crescents and whether that is really a cavitation or I need a new monitor. The dense infiltrates are less typical of PCP. Bacterial agents would still be a possibility. It all seems too fast for more "chronic" agents such as TB, Nocardia and similar stuff.
As far as non-infectious etiologies, he did not have a BMT so GVHD and other specific conditions like that would not be a concern.
Pulmonary hemorrhage may happen in this patients fairly early. Non-cardiogenic pulm edema would usually be more temporally related to transfusions and the CxR does not seem typical.
Pulmonary chemo toxicity is possible, especially if something like Bleomycin was part of the conditioning regimen and he has been on high O2 flow but would not explain the fever.
I would start antifungals, get a CT scan and, depending on the CT, consider a bronch, CT-guided or surgical Bx.
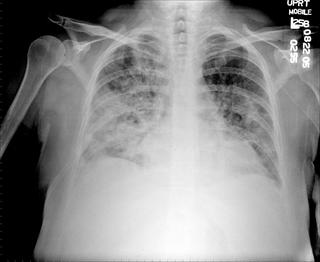
The next day his CXR worsened and his WBC was now 85,000.
Are those blasts or mature WBCs?
The cells were monocytes. They are both mature and immature. It is diagnosed on smear now as chronic myelomonocytic and acute leukemia. (BM Bx pre was AML - M4). Her WBC was 194k and now is 139 after chemo. Now, after the above info, what is your ddx on the CXR findings(BTW the patient is on very broad spectrum abx including 2 antifungals).
Leukostasis or leukoaglutination (am I missing a g?) occurs at counts over 100K and can present with non-cardiogenic pulm edema and quite a lot of pulmonary inflammation. I am a bit confused by the time fram since the infiltrates seem to precede the higher counts... maybe as the WBCs recovered they started getting trapped in the pulm vasculature...
M3's are notorious for DIC during induction and are at high risk for everything from PE's to DAH. M4 is less typical to cause this.
Leukapheresis should be considered.
BTW, did you do a CT scan?
You have the same thoughts. We think the xray findings are indicative of leukostasis at the level of the capillaries, leading to lung injury and non-cardiac pulmonary edema. The xrays and the white count DO in fact go with this; the interesting thing is that it bacame radiographically-apparent at about 85,000. The fact that he is on every antibiotic known to man and still has progression, makes infection with ARDS much less likely. ID service wants a bronch, god bless them. As for plasmapharesis, the same thought as you; but hematology feels that this will not work because of the proportion of *mature* monocytes and apparently it is not effective for this type.
Well... how about some steroids if leukapheresis is out? Any role for that?
The hematologist should have started hydroxyuria to help reduce the WBC count acutely when you patient was trending up (i.e. around 85K).
Also, what is the patient's serum viscosity. If he is having "sludging" in his lung, I imagine that he is having sludging in his vessels elsewhere (i.e. gut, CNS, etc).
Post a Commenttest post a comment