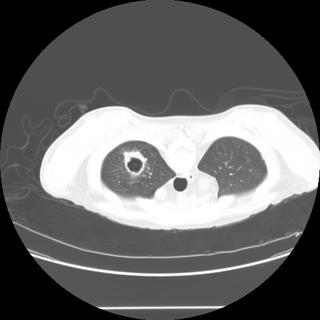
 HC from Michigan has this question: "This gentleman 4 months s/p kidney transplant complaints of shortness of breath. No sputum production. PPD negative pre-transplant. Unable to obtain induced sputums. He had a CT guided biopsy (ID service, before he got to us), of the abnormal finding on CT of the thorax which is negative for AFB and other organisms. Can you reliably rule-out tuberculosis on these grounds without a respiratory sample?; The classic thick vs thin cavity differential diagnosis, can be applied on this case? What is the next step?"
HC from Michigan has this question: "This gentleman 4 months s/p kidney transplant complaints of shortness of breath. No sputum production. PPD negative pre-transplant. Unable to obtain induced sputums. He had a CT guided biopsy (ID service, before he got to us), of the abnormal finding on CT of the thorax which is negative for AFB and other organisms. Can you reliably rule-out tuberculosis on these grounds without a respiratory sample?; The classic thick vs thin cavity differential diagnosis, can be applied on this case? What is the next step?"
Monday, August 15, 2005
RUL cavitary lesion.
 HC from Michigan has this question: "This gentleman 4 months s/p kidney transplant complaints of shortness of breath. No sputum production. PPD negative pre-transplant. Unable to obtain induced sputums. He had a CT guided biopsy (ID service, before he got to us), of the abnormal finding on CT of the thorax which is negative for AFB and other organisms. Can you reliably rule-out tuberculosis on these grounds without a respiratory sample?; The classic thick vs thin cavity differential diagnosis, can be applied on this case? What is the next step?"
HC from Michigan has this question: "This gentleman 4 months s/p kidney transplant complaints of shortness of breath. No sputum production. PPD negative pre-transplant. Unable to obtain induced sputums. He had a CT guided biopsy (ID service, before he got to us), of the abnormal finding on CT of the thorax which is negative for AFB and other organisms. Can you reliably rule-out tuberculosis on these grounds without a respiratory sample?; The classic thick vs thin cavity differential diagnosis, can be applied on this case? What is the next step?"
Subscribe to:
Post Comments (Atom)
3 comments - CLICK HERE to read & add your own!:
I would not stop there because the Bx did not provide you with an alternative Dx to explain the problem. TB is still a concern but there are several other agents (nocardia, Rhodococcus, non-tuberculous Mycobacteria) that can present with an upper lobe cavity in an immunosuppressed patient. Malignancy can also look like that but the Bx should have been diagnostic.
I would consider a bronch with BAL and TBBx of the area.
Is he very symptomatic (cough, fevers, etc.)?
I agree, and think that Nocardia would be a primary concern here. Prior to bronchoscopy, I would do a head CT, as this would increase my suspicion of Nocardia.
I would follow that with a bronch, and specify to the micro department that you are looking for Nocardia, atypical mycobacteria, Rhodococcus, etc.
Post a Commenttest post a comment