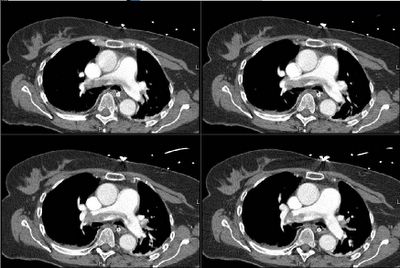
This has come up today: we have been following this 59 y/o woman on the neurosurgery service. She presented with HTN crisis with a hemorrhagic CVA and has been fairly stable. She has had SCDs on. Tody she had an increase in FiO2 requirements and became more tachycardic. No hypotension. No CP. I got a CT angio that looks as follows.
What would you do next?
The follow-up to this case is posted above on this link.
Subscribe to:
Post Comments (Atom)
3 comments - CLICK HERE to read & add your own!:
Well, she has a saddle embolism so the question is what should you do? She is hemodynamically stable (suggesting no right heart failure), so unless she has refractory hypoxia, embolectomy would not be necessarily be indicated. However, because this is a saddle embolus, the question becomes, do you put in an IVC filter and anticoagulate? IVC filters plus anticoagulation reduces the risk of recurrent PE from 8.6% to 1.1% (N Engl J Med 1998;338:409-15), so if there is high risk of death if there were o be a second PE, this might be considered. Also, I just realized - oops- that she had a hemorrhagic CVA so the filter is a must because she can't be anticoagulated. I think that with CVA-hemorrhage from HTN emergency, the anticoagultion can be started latr down the road if the BP is controlled.
Yes, she has a large saddle embolus AND a hemorrhagic CVA. She is a bit hypoxemic but not refractory, she improves with higher flow O2. She needs a filter but with the CVA is there anything else to do? Our radiologists here don't do catheter embolectomies.
She still has a drain and some blood in the ventricles so the neurosurgeon is not too keen on anticoagulation yet.
I think that's the key-the neurosurgeon doesn't think it's safe. This is the proverbial stuck between a rock and a hard place. There is no indication for surgical or catheter embolectomy and, as it turns out, there is very little data supporting a benefit for these procedures. Nevertheless, if she were to deteriorate from here, I see no other option (as obviously thrombolytics are contraindicates).
So, I'd place hte filter and hope for the best, although this may be a situation to consider the preemptive transfer to "an academic institution" with the capability for intervention should the need arise.
Post a Commenttest post a comment